Last week, I co-wrote an article with Joan Saba, a partner at the architecture firm NBBJ, on how we can build more resilient communities by combining the ideas of architecture and public health. With hurricane season underway, the need for such resilience has rarely been more apparent. As I write this note, Hurricane Florence approaches the Carolinas and news reports warn of the storm’s potential destructiveness. These reports come almost exactly one year after Hurricane Maria showed us how devastating such storms can be. Whether Florence will approach Maria’s devastation is a question to be answered by time, hopefully in the negative. However, whether or not the Carolinas—or any region—have the resilience to absorb and recover from a disaster like a hurricane is a question we can indeed answer now.
That answer lies in whether or not we design our communities and urban spaces with resilience in mind. Extreme weather events, driven by climate change, have made the need for such design more urgent with each passing year.
As shown in Figure 1 below, the incidence of natural disasters is increasing worldwide. Several factors are driving this observation, including rising sea temperatures, more media coverage of disasters throughout the world, and improvements in measuring weather events over time.
Figure 1.
Number of natural disasters worldwide, 1980-2010. Adapted from: Munich Re (2010) “Topics Geo natural catastrophes 2009: Analyses, assessments, positions.” Munich: Munich Reinsurance Company, by Jennings, S. “Time’s Bitter Flood: Trends in the number of reported natural disasters.” Oxfam Research Report 2011.
Recognizing, as noted above, the mental and physical health consequences of disasters, the central question for this note is: How can a city mitigate these potential consequences?
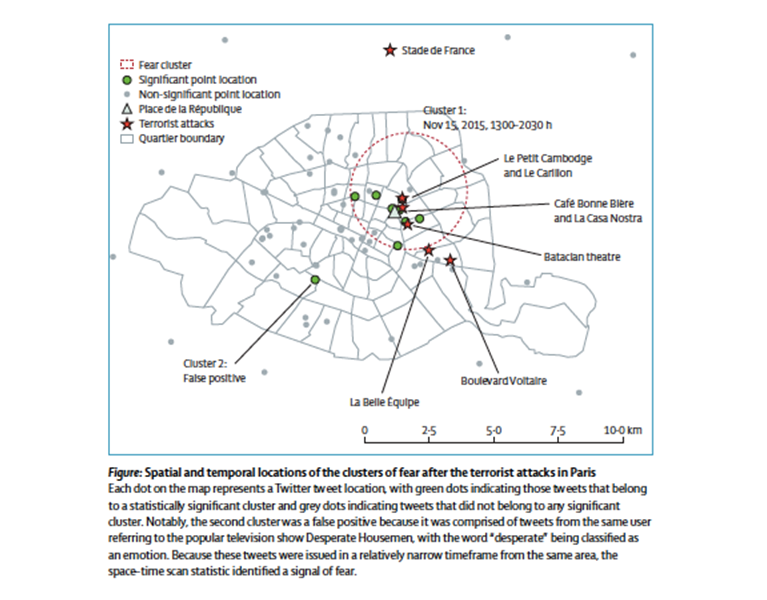
First, through an awareness of risks. One of the challenges inherent in anticipating disasters is readiness. Unfortunately, disasters all too often seem to arise unexpectedly. While we have a relatively limited capacity to anticipate when most disasters will strike, we do reliably know that disasters will happen, and that areas characterized by particular geologic and meteorological features are especially at risk of these events. This suggests that cities’ awareness of risks, and planning for potentially catastrophic events, are central to the resilience of urban areas. Such planning entails cities keeping up-to-date maps of resources that may be of use during times of crisis, including different domains of health care or information technology throughout the city. Such inventories can also draw attention to areas of vulnerability, including particular geographic areas prone to flooding. Active surveillance networks can then report on threats in real time, in the context of this system. This approach may guide response to particular hotspots of disease burden following disaster—in a paper we demonstrated the role that active surveillance can play in detecting the health consequences of large-scale events (Figure 2).
Figure 2.
Gruebner O, Sykora M, Lowe SR, Shankardass K, Trinquart L, Jackson T, Subramanian SV, Galea S. Mental health surveillance after the terrorist attacks in Paris. The Lancet. 2016;387: 2195-2196.
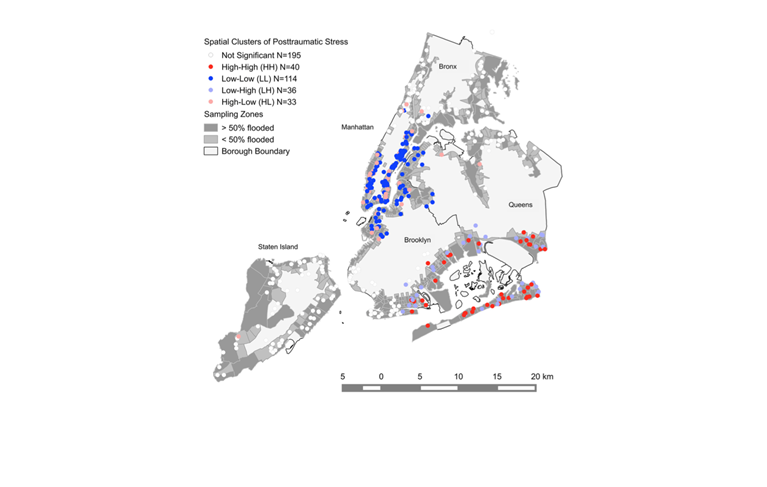
Second, cities need to be responsive in a range of capacities, with an infrastructure that can address a broad variety of challenges. An example of this type of diversity lies in strong, flexible primary care clinics or community health centers. These clinics receive patients as the first point of contact during a disaster, and launch systematic investigations into potentially new health threats, leading to quicker recognition of emerging epidemics, as well as greater satisfaction and trust in the system on the part of the public. This system functions best where universal health coverage is in place, so that lower-income families—especially vulnerable in times of disaster—can receive the care they need in the event of an emergency. The map below (Figure 3), shows clusters of post-traumatic stress symptoms following Hurricane Sandy in New York City. It is not surprising that the Far Rockaways and surrounding area saw heavy symptom clusters (red dots shown), given the extent of damage in that area. Lower Manhattan and Staten Island were also hit badly, as one can see by the gray shading, but they did not have the same clustering of high symptoms; it could be that those parts of the city had resources that the rest of the city lacked post-disaster.
Figure 3.
Significant spatial clusters of Posttraumatic Stress in New York City after Hurricane Sandy. Gruebner O, Lowe SR, Sampson L, Galea S. The geography of post-disaster mental health: Spatial patterning of psychological vulnerability and resilience in New York City after Hurricane Sandy. International Journal of Health Geographics 2015; 14:16.
Third, resilient cities can successfully contain and isolate health threats while still delivering core services, which keeps non-affected residents healthy so that the effect of the threat on areas of life like education or occupational productivity is lessened. Self-regulation requires long-term investment in infrastructure—in the core economic and structural conditions that promote healthy populations. An exclusive focus on emergency response, to the detriment of an investment in core infrastructure, stands to expose populations to undue risk, relying on a post-event curative approach, rather than a preventive approach that invests in robust populations.
Fourth, resilient cities need to have integrated systems that can respond jointly. Communication should be clear across different sectors, sectors like public health and health care—not an easy task. Funds may need to be shared or reassigned, and the private sector needs to work with the public sector. Further, communities should not be seen simply as recipients of care, but as actors in the health system. One effective example of integration in a health system is LifeNet, a 24/7, multicultural crisis center in New York City that emerged in the aftermath of the September 11, 2001, terrorist attacks. LifeNet offers free behavioral health assessments in multiple languages, and connects both providers and patients with service information and resources.
Fifth, resilient cities are adaptive; they can readily transform, both in times of challenging conditions and under normal circumstances. This allows them to improve function and keep a flexible organizational structure with strong leadership. After a disaster has passed, the adaptive health system ideally functions better than before the disaster; the idea is not just to fix the problem at hand but also to become more efficient and productive in the long run. Research of past crises is therefore crucial in guiding how cities may become more adaptive in the aftermath of a disaster.
Unfortunately, natural and other disasters will continue to occur. A 2015 article in The New Yorker about an impending earthquake in the Pacific Northwest asked, “How should a society respond to a looming crisis of uncertain timing but of catastrophic proportions? How can it begin to right itself when its entire infrastructure and culture developed in a way that leaves it profoundly vulnerable to natural disaster?” This was the most downloaded piece in the magazine that year; it well highlighted many of the limitations we face in the US in planning for disasters. To answer its question: In order to safeguard population health, cities must have a disaster response plan in place, as well as a strong infrastructure that can support both daily stressors and the sudden catastrophes that are unfortunately always liable to occur anywhere, anytime.
I hope everyone has a terrific week. Until next week.
Warm regards,
Sandro
Acknowledgement: I am grateful for the contributions of Laura Sampson to this Dean’s Note.